I am the Director of Clinical Education for a Master’s in Speech-Language Therapy programme at The University of Auckland, New Zealand, where I provide both classroom teaching and clinical education. I am a practising Speech-Language Therapist and enjoy engaging in research into supervision and clinical education innovations. I also provide supervision training and have recently submitted my PhD, which explored the speaking up experiences of allied health new graduates.
You can follow me on LinkedIn: linkedin.com/in/philippa-m-friary-a74a2143
‘I know what I want to say … but I don’t know if I can say it or how to say it?!’ This was a quote taken from an interview I had with a new graduate in allied health who was working within a large metropolitan hospital in Aotearoa, New Zealand. This interview was one of many completed as part of my doctoral study titled: Speaking up in healthcare – an exploration of allied health new graduates’ experiences of speaking up.
You may be wondering about the link between speaking up and supervision. A key outcome from this two-phase realist informed study was that relational and reflective supervision has a beneficial impact on the speaking up skills of new graduates in allied health. From my doctoral study, I developed R.O.A.R. – supervision for speaking up – a framework that supports supervisors in ensuring that their supervision practice supports the speaking up knowledge and skills of supervisees. Therefore, promoting the development of a healthy speaking up culture in our workplaces – something we are all responsible for. In this two-part blog, part 1 will provide a brief background to the topic – speaking up, and a summary of the study that underpins this framework. Part 2 will introduce you to R.O.A.R. – the supervision framework for speaking up.
Promoting effective speaking up skills across all sectors of the healthcare workforce is a cost-effective way to improve quality and safety in healthcare. Despite national reports and literature identifying the importance of speaking up (Carroll & Edmondson, 2002; Detert & Edmondson, 2011; Edmondson, 2018; Health Quality & Safety Commission, 2016; Wilkinson et al., 2024), staff continue to not speak up across many workforce sectors (Morrison, 2014, 2023). Ineffective speaking up or withholding voice impacts patient safety and stifles quality improvement. Left unexamined, this behaviour can exacerbate and form a culture of silence across healthcare settings (Morrison, 2023). Any targeted intervention to improve the speaking up culture in healthcare will only be effective with an in-depth understanding of the speaking up experiences of all workforce sectors. While speaking up has been explored in nursing and medicine and workforce groups outside of healthcare, this knowledge does not apply to allied health workers, particularly new graduates in allied health.
In a scoping review I completed looking at speaking up in healthcare, 76 articles were examined between 2009 and 2019. Only three studies included qualified allied health participants (Pharmacy and Dentistry), and no studies reported on allied health new graduates. While some researchers report the need for more cross-pollination of research across different sectors and research fields (Morrison, 2023; Wilkinson et al., 2020), I argue that new graduate allied health workers have different roles and responsibilities and professional culture compared to nursing and medicine and therefore require a separate research focus.
The overall aim of this doctoral study was to answer the question: what are the experiences of new graduates in allied health in speaking up in healthcare?
This question was examined in-depth through the following specific questions:
(1) How do new graduates in allied health experience speaking up about quality improvement and patient safety?
(2) What features of the context and what causal mechanisms influence this behaviour?
(3) How does their experience of speaking up change over 1 year?
To explore these questions, a two-phase realist-informed research project was conducted employing both realist and narrative analysis methods. Phase 1 included four different focus groups, two involving new graduates in allied health and two involving supervisors of new graduates in allied health. These participants worked within one of three large hospitals in Aotearoa, New Zealand. Phase 2 was a longitudinal interview study exploring speaking up over time with a cohort of 10 allied health new graduates also working within healthcare settings in a large metropolitan hospital in Aotearoa, New Zealand.
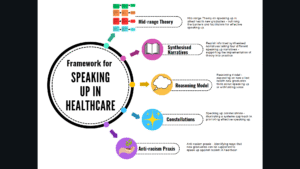
Findings have been developed into an Education and Practice Framework for Speaking Up in Healthcare. This framework provides information and pragmatic recommendations that will support new graduates, supervisors of new graduates, healthcare educators, leaders and organisations to further develop a healthy speaking up culture in their workplace.
This study uncovered that these new graduates had not received any training in speaking up. Some shared stories of effective speaking up, and many shared stories in which they did not speak up or did so ineffectively. And over time, it was evident that these new graduates were speaking up less as they socialised into the hospital system. Those who shared stories of effective speaking up highlighted the role that quality supervision had in developing, preparing for and debriefing on this communication exchange. Part 2 will unpack the supervision elements that promote effective speaking up – R.O.A.R. – supervision for speaking up.
By Philippa M. Friary